⏰ Last Update: 14.08.2024
Rheumatism is a general and non-specific term that is often used to describe symptoms associated with a broad category of conditions that affect the joints or connective tissues. These conditions cause chronic, often intermittent pain that affects the joints, tendons, ligaments, bones, and muscles. In this article, we will delve into the intricacies of rheumatism, discussing its causes, symptoms, and available treatment options.
Understanding Rheumatism
Traditionally, the term “rheumatism” was utilized as a broad descriptor for a range of conditions characterized by symptoms affecting the musculoskeletal system. These conditions primarily include a spectrum of inflammatory disorders that impact the joints, muscles, tendons, ligaments, and bones. However, with advancements in medical science and a clearer understanding of these conditions, the usage of the term “rheumatism” has become less frequent in modern clinical language.
Arthritis
Arthritis, encompassing over 100 different types, is the most common rheumatic condition. The term “arthritis” literally translates to joint inflammation, and it’s characterized by pain, stiffness, swelling, and potential deformity in one or more joints.
Rheumatoid arthritis
One of the most prevalent forms of arthritis is rheumatoid arthritis (RA). RA is an autoimmune disease where the body’s immune system mistakenly attacks its own tissues, primarily affecting the lining of the joints. This leads to chronic inflammation and can result in joint damage, deformity, and loss of function.
Osteoarthritis
Another commonly recognized condition in the family of rheumatic diseases is osteoarthritis (OA). Unlike rheumatoid arthritis, osteoarthritis is primarily a degenerative joint disease that results from wear and tear over time, often affecting the hands, knees, hips, and spine. It’s characterized by the breakdown of cartilage that cushions the ends of bones in joints, causing bones to rub together and resulting in pain and stiffness.
Lupus
Lupus, another autoimmune disorder, also falls under the umbrella of rheumatic conditions. This condition can affect various body systems, including joints, skin, kidneys, blood cells, brain, heart, and lungs. It’s characterized by periods of illness, called flares, and periods of wellness, or remission.
Fibromyalgia
Fibromyalgia, another condition typically classified under rheumatic diseases, is characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and memory and mood issues. While it’s believed to amplify painful sensations by affecting the way your brain and spinal cord process pain signals, the exact cause remains unknown.
Each of these conditions, while categorized under the wider umbrella of “rheumatism,” exhibits unique characteristics and requires specific treatment strategies. This specificity is why modern medical terminology tends to favor these individual names over the generalized term “rheumatism.” Nevertheless, all these conditions share a common focus on maintaining and improving joint health and mobility and managing pain and inflammation.
Causes of Rheumatism
Rheumatic conditions are complex and multifactorial, and their causes are not entirely understood. However, they generally stem from one or more of the following factors: inflammation, wear and tear of joint tissues, and autoimmune reactions. Here’s a more detailed look at each of these contributing elements:
Inflammation
Many rheumatic diseases are inflammatory conditions, meaning they are characterized by inflammation in one or more parts of the body. Inflammation is a physiological response to injury or disease, which, in normal circumstances, helps the body to heal. However, in rheumatic conditions, inflammation often occurs inappropriately or becomes chronic, leading to pain, swelling, and tissue damage.
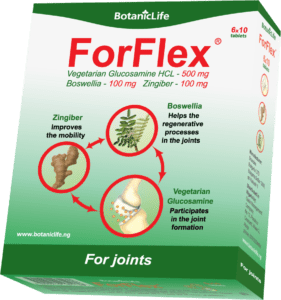
Ginger and boswellia are herbs that are well-known for they anti-inflammatory actions. They are both available in the forms of high quality extracts in ForFlex: https://botaniclife.ng/product/forflex/
Wear and Tear
Some rheumatic diseases, most notably osteoarthritis, are primarily caused by the gradual wear and tear of joint tissues, particularly cartilage. Over time, repetitive use of joints can cause the protective cartilage that cushions the ends of bones to deteriorate, leading to bone rubbing against bone, which results in pain and stiffness.
Autoimmune Reactions
Many rheumatic conditions, including rheumatoid arthritis and lupus, are autoimmune disorders. This means that the body’s immune system mistakenly attacks its own tissues, causing inflammation and damage. In the case of rheumatoid arthritis, for instance, the immune system primarily targets the lining of the joints, causing chronic inflammation and potentially severe joint damage.
Genetic Factors
Certain rheumatic conditions have a genetic component, making them more likely to occur in individuals who have a family history of the disease. This is particularly true for diseases like rheumatoid arthritis and lupus.
Age
Age is a significant risk factor for many rheumatic conditions. As the body ages, the cartilage in the joints can become more susceptible to wear and tear, making conditions like osteoarthritis more common in older adults.
Obesity
Carrying extra weight puts additional pressure on joints, particularly those in the knees, hips, and lower back, increasing the risk of wear and tear. Obesity can also trigger inflammation in the body, which can contribute to the development of some rheumatic conditions.
Infections and Physical Trauma
Certain infections can trigger or exacerbate some rheumatic diseases, while physical trauma to a joint, perhaps due to a sports injury or accident, can sometimes lead to the development of a rheumatic condition later in life.
Understanding these causative factors is key to the prevention, management, and treatment of rheumatic conditions. It’s important to note that these factors often interact, and a combination of several of them may be involved in the onset of a rheumatic condition.
Symptoms of Rheumatism
The symptoms of rheumatic conditions vary depending on the specific disease. However, common symptoms include:
- Joint pain and stiffness.
- Swelling in one or more joints.
- Reduced range of motion in the affected joints.
- Persistent fatigue.
- Fever associated with other symptoms.
- The presence of rheumatoid nodules, which are firm lumps under the skin.
- Symptoms affecting other body systems, such as the eyes, lungs, heart, and nerves, particularly in conditions like rheumatoid arthritis and lupus.
Diagnosis of Rheumatism
Diagnosis usually involves a comprehensive physical exam, patient history, and various tests, including blood tests, X-rays, and MRI scans. These tests help doctors determine the type and extent of the rheumatic disease and inform the most suitable treatment approach.
Treatment of Rheumatism
Rheumatic conditions are often chronic and require long-term management strategies to control symptoms, slow the disease’s progression, and improve the patient’s quality of life. The choice of treatment usually depends on the type and severity of the condition, the patient’s overall health, and their personal needs and preferences. Here are some of the most common approaches:
Medications
The cornerstone of rheumatism treatment involves medications that can help control inflammation, relieve pain, and slow the disease’s progression. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce inflammation and alleviate pain. Corticosteroids provide potent anti-inflammatory effects and can be used for short-term relief during severe flare-ups. Disease-modifying antirheumatic drugs (DMARDs), including both conventional and biologic DMARDs, are often used in conditions like rheumatoid arthritis to slow disease progression and prevent long-term damage to the joints.
Physical Therapy
Working with a physical therapist can be beneficial for patients with rheumatic conditions. They can devise individualized exercise plans to maintain or improve mobility, strengthen muscles supporting the affected joints, and enhance overall physical function. Physical therapists can also offer advice on how to protect joints from further damage.
Lifestyle Modifications
Lifestyle changes are often crucial in managing rheumatic conditions. Regular, gentle exercise helps keep joints flexible and strengthens the muscles that support them. A balanced, nutritious diet can support overall health and assist in maintaining a healthy weight, which can alleviate stress on weight-bearing joints. Habits like smoking or excessive alcohol consumption, which can exacerbate inflammation, should be avoided.
Surgery
For patients with severe rheumatism that doesn’t respond to other treatments, surgery may be an option. Procedures can range from arthroscopy (a minimally invasive surgery to remove or repair damaged joint tissue) to joint replacement surgery, where a damaged joint is replaced with an artificial one. These options can dramatically improve quality of life for some patients.
ForFlex
Beyond these traditional methods of treatment, natural supplements like ForFlex can be an advantageous part of a comprehensive rheumatism management plan. ForFlex is a supplement formulated to support joint health and mobility. Its key ingredients work synergistically to promote joint flexibility, reduce inflammation, and offer antioxidant protection. Learn more about ForFlex on the following link: https://botaniclife.ng/product/forflex/
Remember that rheumatic conditions often require a multifaceted approach to treatment. Regular medical check-ups are necessary to monitor the disease’s progression and adjust treatment plans as needed. With the right approach, it’s entirely possible to lead an active, fulfilling life despite a rheumatic condition.
Conclusion
Rheumatism represents a range of conditions that can cause significant pain and disability. However, understanding these diseases and the options available for their management can help those affected lead fulfilling lives. It is always recommended to consult with a healthcare provider for an accurate diagnosis and personalized treatment plan. Regular check-ups and a proactive approach to overall health can also play a vital role in managing rheumatic conditions.